New policies and practices suggested for avoiding RSIs

Studies have estimated the incidence of retained surgical items (RSIs) as one in 5,500 to one in 6,975 cases. In October 2013, The Joint Commission issued a Sentinel Event Alert on RSIs, and periodic reports in the media have raised the public’s awareness of this persistent problem.
Effective policies, reliable practices, ongoing education, and other initiatives can reduce the risk of an RSI. OR Manager spoke with leaders at several different facilities who have taken innovative approaches to the problem.
A multistakeholder effort is essential for developing a policy related to RSIs, says Verna Gibbs, MD, clinical professor of surgery at the University of California at San Francisco and founder of NoThing Left Behind®, a national surgical patient safety project to prevent RSIs.
“It’s not just about what the nurses are supposed to do. It’s nurses, surgeons, surgical technologists, anesthesiologists, radiologists, and radiology technologists—because all those people are team members and should be held accountable,” Dr Gibbs explains, adding that representatives from labor and delivery should be part of the discussion as well.
This collaboration can help identify simple changes that are needed. At one hospital, for instance, the radiology technicians realized they didn’t know which images they needed to take when the team was looking for a missing item or how many images were needed.
“It was great to cross that divide and understand what they were dealing with and what the problem was as seen from their eyes,” Dr Gibbs says.
Not all policies are created equal. “A good policy has directive actions and doesn’t rely on people making up their minds,” Dr Gibbs says. For example, a policy that states, “Sponges will be counted in all cases when there is a chance of retention” isn’t a good policy.
“How are you going to determine whether there is a chance that a sponge will be retained?” Dr Gibbs asks. For example, there have been incidents of retained sponges with small cases—procedures generally regarded as having little chance for retention.
“You shouldn’t have judgment in policies,” she adds. “The policies are supposed to direct the individual to action. If they can’t, then tell the person what to do to resolve the problem using the ‘if this, then that’ format.” For instance, if a final sponge count is incorrect, the nurse must complete an incident report in the electronic system.
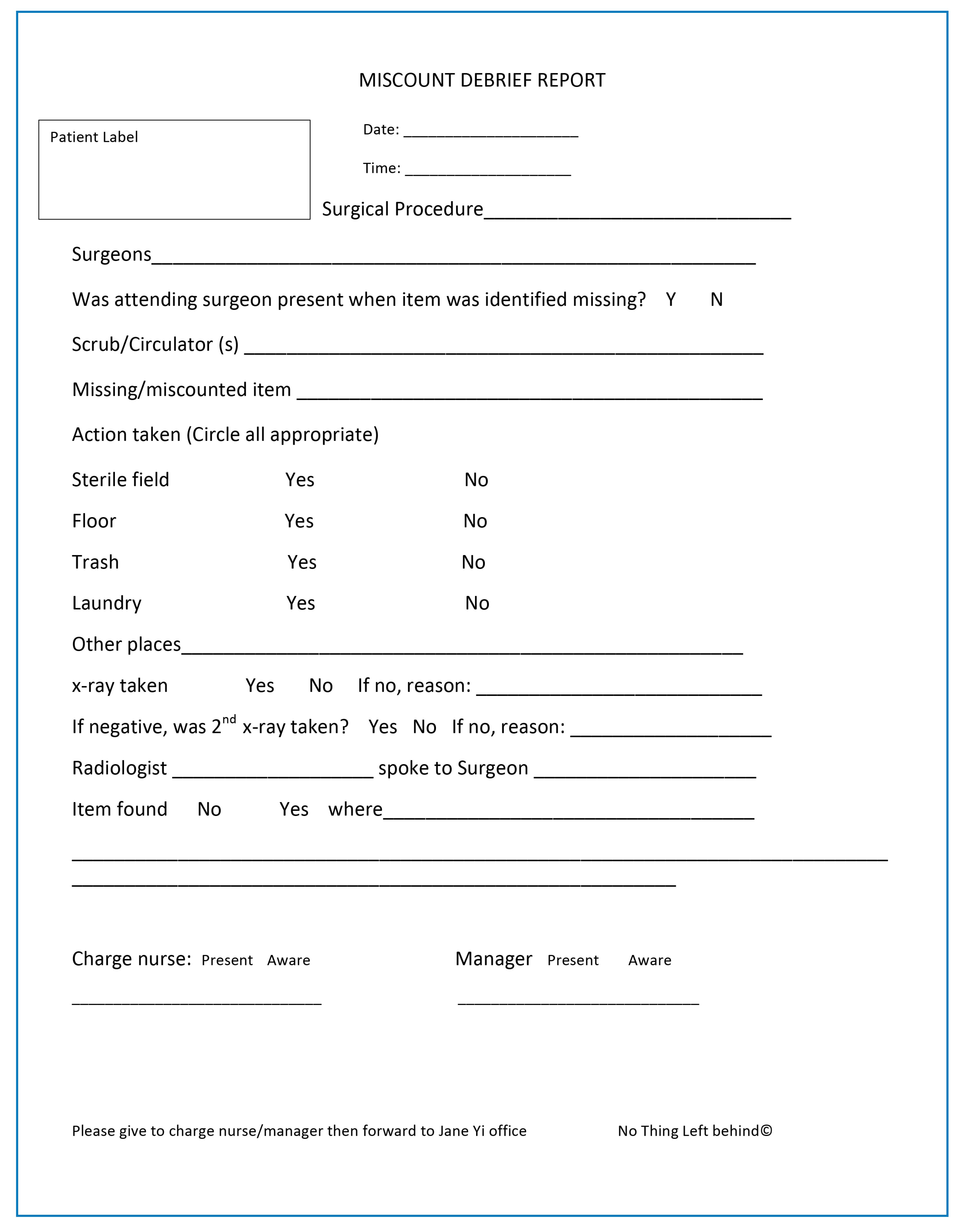
Completing a near-miss report every time a miscount occurs and sharing these reports helps OR teams understand where practice problems occur. Courtesy of Verna C. Gibbs, MD. Used with permission.
Completing a near-miss report every time a miscount occurs and sharing these reports helps OR teams understand where practice problems occur. Courtesy of Verna C. Gibbs, MD. Used with permission.

Dr Gibbs has developed the “NoThing Left Behind®: Prevention of Retained Surgical Items Multi-Stakeholder Policy” by working with various entities. OR managers who want to use this policy at their organization may obtain a PDF of the policy at http://www.nothingleftbehind.org/uploads/NoThing_Left_Behind_Policy_v5.pdf or request a Word document from Dr Gibbs at [email protected].
She emphasizes the need to use the entire policy and not simply incorporate isolated phrases into the organization’s own policy. “This isn’t a menu where you can take one from column A and one from column B,” she says. “The policy has strong internal consistency.”
Dr Gibbs found that by taking the piecemeal approach, one hospital ended up with three different ways nurses could manage sponges all in one policy. “You don’t want to contradict what you say in one part of your policy with what you say in another.”
The Multi-Stakeholder Policy was revised in early 2015, and Dr Gibbs summarizes some of the changes.
Therapeutic packing. “People are still having trouble understanding this process,” Dr Gibbs says. Therapeutic packing should not be reported as an episode of an RSI. “Therapeutic packing is not a reportable case of retention,” she says. The policy recommends using lap sponges for abdominal packing because they are easily available and detectable by x-ray. It’s also not required to know exactly how many sponges have been used to pack because under circumstances when therapeutic packing is used, much uncertainty usually exists.
“It doesn’t matter how many go in, what’s important is that the team makes sure that all the sponges are out of the patient at the time of the final wound closure,” she says.
When the patient returns for wound closure, the packed sponges should be placed in separate holders, and before closure, two different x-ray views should be taken and read by a radiologist to verify there are no lap pads in the patient.
Instruments. Dr Gibbs says a recurring question has been, “Do we have to count all these instruments in all these cases?” The revised policy clarifies that counting is just one strategy—not the only strategy—for ensuring items are not left in the patient.
An alternative strategy is to have the surgeon perform the methodical wound exam with the scrub person performing a back table and field exam; together, they can determine if an instrument is inside the patient. A standardized back table works well for all operations because it can help the scrub person know when something is missing.
Counts. AORN’s recommended practices state that a count should be completed “at skin closure at the end of the procedure or at the end of the procedure when counted items are no longer in use (ie, final count).”
Dr Gibbs says nurses find this confusing. “The wording is very problematic because of the ‘or’ in the middle of the sentence. This is a huge driver of bad practice and fuzzy thinking.” She adds that a way to provide clarity to the statement is to write it as two separate directives: “A count should be performed when skin closure begins. A count should be performed when all items are no longer in use (ie, final count).”
In the Sponge ACCOUNTing System (SAS), the final sponge count is defined as when all the sponges (the used and unused sponges) are in the hanging blue-backed sponge holders. “You can’t have sponges on the field and call it a correct final count,” Dr Gibbs says. (For more information on SAS, see http://www.nothingleftbehind.org/Sponge_Accounting.html.)
The revised Multi-Stakeholder Policy emphasizes that counts be performed “from out to in.” Start with what is on the dry erase board, in the sponge holders, off the back table, on the back table, on the Mayo stand, on the surgical field, and what is in the incision. Counting from the opposite direction can lead to errors because, for example, people count the malleable retractor being used in the incision as accounted for even though it’s still in the patient when counting from “in to out.” This problem has been a contributing factor in retained malleable retractor cases and is probably the primary reason this retractor is the most commonly retained instrument.

Committees are helpful for ongoing assessment of ways to reduce the risk of RSIs and for crafting policies. Thanks to the efforts of the Count Process Improvement Committee at Stanford Hospital & Clinics, Stanford, California, the number of retained items went from one per month for about 6 months to none in 2013, and there was only one RSI incident in 2014.
“We are constantly looking at what’s going on with counts,” says Sharon L Butler, MSN, RN, clinical nurse IV, who has chaired the committee since 2009. “It helps us identify trends and stay on top of any potential problems.”
The Stanford committee, which meets monthly to review risk reports, has 12 members, including a manager, an assistant manager for quality in the OR, educators (one from the inpatient OR and one from ambulatory surgery), and staff.
“Committee members bring back issues they have identified in their practice areas,” Butler says. The committee strategizes about how to best resolve those issues.
The committee also identifies best practices. For example, based on the committee’s recommendation, the OR team now removes all 4 x 4 sponges from the surgical area when closure of the surgical incision starts.
Butler notes that some hospitals also remove lap sponges, but Stanford has chosen not to do so, relying on x-rays as needed instead. The focus on reducing RSIs has even changed physician practice. “Some surgeons want to only use lap sponges and not Raytec sponges,” Butler says.
Other changes the committee has made include:
- Using blue-backed plastic sponge holders
- Reestablishing the baseline count for all items except instruments in two-part procedures where the patient is repositioned, reprepped, and redraped
- Implementing mandatory x-rays in specific situations (sidebar, p 7)
- Creating a new audit tool for monitoring staff compliance to procedure
- Implementing use of a miscount report (sidebar, p 8)
- Tracking items that are intentionally left in place and ensuring these items are x-ray detectable, if possible. Nurses use the electronic health record to document when these items are left in and when they are removed.
Changes that involve surgeons are first reviewed and approved by the chiefs of surgery committee.

Sharon L. Butler, MSN, RN
Sharon L. Butler, MSN, RN

Adam Royer, MS, BSN, CNOR
Adam Royer, MS, BSN, CNOR
One of the challenges of teaching staff about RSIs is overcoming the “it won’t happen to me” mentality, says Adam Royer, MS, BSN, CNOR, administrator of surgical services at Erlanger Health System, Chattanooga, Tennessee.
When the OR staff identified the problem of retained items that were caught before the patient left the OR, Royer says they followed the standard of creating a team, examining processes, and implementing change. When it came to education, however, the team turned to a tool long used by surgeons—morbidity and mortality (M&M) rounds.
A surgeon experienced in M&M rounds presented cases where a retained item would have occurred if processes such as obtaining an x-ray had not been followed. The key was that all the cases occurred at Erlanger, and the surgeon had the x-rays to demonstrate the case to the nurses, surgical technologists, and anesthesia providers who attended the 1-hour session, Royer explains.
“We didn’t just tell them it could happen, we showed them it can happen,” Royer says. For instance, staff questioned the need to count a retracting ratchet because it isn’t placed in the patient’s body, but Royer says x-ray evidence showed, “It happened with us in the OR with people they work with every day.”
Although some physicians didn’t want their cases presented, Royer says, the chief of surgery stood up for the initiative. M&M rounds allowed an open discussion in a safe environment about possible system failures.
Two years after the initial program, a quality improvement analysis found a decrease in RSIs, zero patients leaving the OR with an RSI, and an increase in the number of x-rays obtained to check for RSIs.
At Stanford, Butler uses the OR’s dedicated Monday morning in-service time to discuss any issues related to counting and RSIs. And frequently a committee member submits an item to the OR’s weekly bulletin. “We use it to share trends and help staff stay on top of what they need to be doing,” she says.
In addition, information on how to avoid RSIs is included in orientation and is part of nurses’ and surgical technologists’ annual competencies.

Use of a plastic hanging blue-backed sponge holder with a defined standardized practice is preferable to counting out of the kick bucket or laying sponges on a sheet on the floor. Some organizations use radiofrequency scanners or bar-code counting devices.
Dr Gibbs notes that technology is not a panacea. Equipment can break, electronic equipment needs to be plugged in, and supplies must be kept at hand. Staff sometimes use devices incorrectly or not at all. In addition, Dr Gibbs says, no matter what technology nurses use, surgeons must do their part and perform a methodical wound exam in every case.
“The anchoring concept about retained surgical sponges is not what the humans use, it’s that the humans have to use something,” Dr Gibbs says. “It doesn’t matter if it’s a cheap, plastic sponge holder or an expensive scanning device with a wand; humans usually fail by not using them because they think that counting is sufficient. Counting alone will not get you to zero.” ❖
Cynthia Saver, MS, RN, is president of CLS Development, Inc., Columbia, Maryland, which provides editorial services to healthcare publications.
Reference
The Joint Commission. Sentinel Event Alert Issue 51: Preventing unintended retained foreign objects. October 17, 2013. http://www.jointcommission.org/sea_issue_51/.
Mandatory x-rays
At Stanford Hospital & Clinics, Stanford, California, the criteria for obtaining a mandatory x-ray are:
- A baseline count was not established (as sometime occurs with emergency surgery).
- The procedure lasts longer than 10 hours and there have been four changes in surgical technologists.
- Therapeutic packing was used (before wound closure) and those items need to be removed.
- The count is incorrect.
Patients who have had liver transplant surgery also receive x-rays even if the count is correct.