OR Manager Conference third place poster winner showcases impactful program from 2023
By Marisa Torrieri
From highlighting the need for better preoperative nasal decolonialization to touting the success of personalized pediatric behavioral health interventions, the posters on display at the 2023 OR Manager Conference highlighted the exceptional work of clinicians in 2023.
Poster: “Use of Alcohol-Based Nasal Antiseptic in Reducing Surgical Site Infections in Patients Undergoing Elective High-Risk Procedures”
Surgical site infections (SSIs) create a financial burden and negatively affect patient outcomes. Vicki Yfantis, MSN, RN, ANP-BC, CPAN, CAPA, clinical director of perioperative services at Suburban Hospital, a member of Johns Hopkins Medicine, Maryland, and her clinical team hoped that a simple intervention would make a big impact on outcomes. The challenge was getting a pilot approved by multiple leaders on multiple teams.
Q: Can you tell us what sparked this interest in the topic of nasal decolonization interventions?
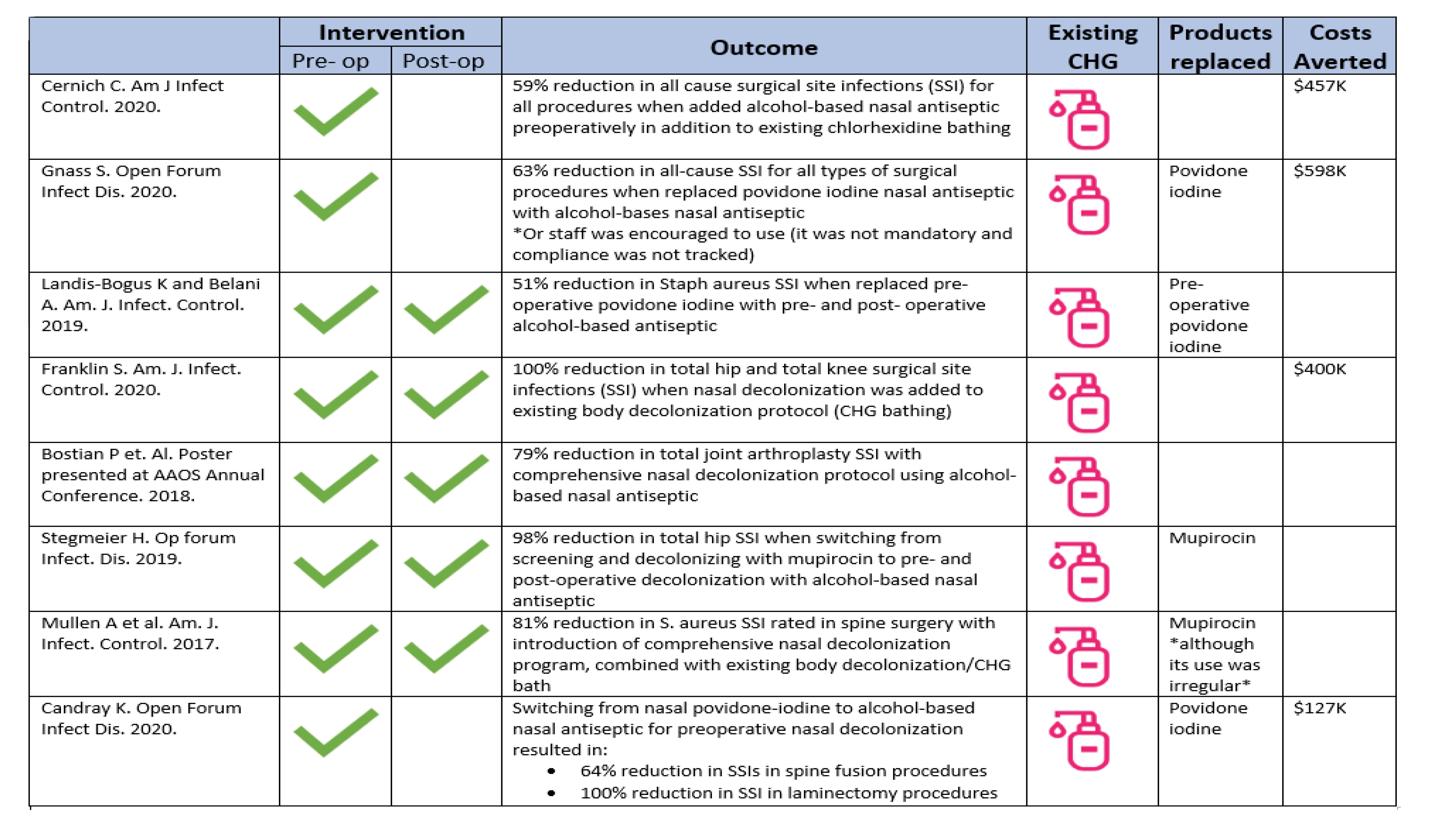
Yfantis: Prepandemic, we noticed an uptick in our SSI numbers. Upon review of our SSI prevention strategies, we noticed an opportunity for improvement in nasal decolonization. The CDC [Centers for Disease Control and Prevention] recommends that all patients undergoing high-risk surgeries (eg, orthopedic, neurosurgery, cardiothoracic), unless known to be S. aureus negative, use an intranasal, anti-staphylococcal antibiotic or antiseptic and CHG wash prior to surgery. Although we had a long-standing practice of implementing CHG bathing for all patients preoperatively, we struggled with consistent nasal decolonization—the main issue being compliance around screening and subsequent treatment for MRSA and MSSA.
The need to increase consistency and compliance with SSI prevention strategies was our main driver, but the inspiration behind our poster was to highlight the successful implementation of a nurse-driven intervention that positively impacted patient outcomes.
Q: Can you break down the details of the pilot?
Yfantis: We noticed that surgical patients were screened too late for MRSA and not getting treated in time, particularly during the pandemic due to COVID-19 testing demands. And those patients who did receive a prescription for MRSA treatment were not compliant.
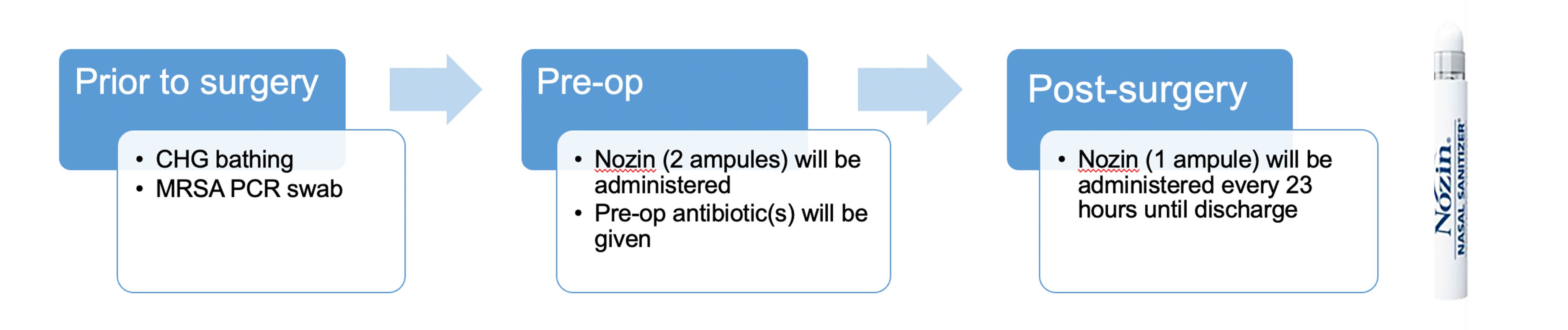
The project team involved members from all phases of perioperative nursing. We researched and decided on a nasal antiseptic to pilot, developed, and disseminated an implementation plan and protocol, including the creation of a non-prescriber-initiated order (NIPO), which was key. The pilot population chosen was patients undergoing total joint arthroplasty and/or all spine surgical procedures.
Prior to surgery, the presurgical testing nurse identifies the patients who fall into the category of needing nasal sanitizer and enters an order into our electronic health record (EHR). When the patient arrives on the day of surgery, the preoperative nurse releases the order in the EHR and administers—or instructs the patient to self-administer—the alcohol-based nasal sanitizer. The beauty of the product we chose is that it does not matter what time the patient administers it, as long as it is before incision. There are no time constraints, and it does not interfere with other SSI prevention strategies.
Postoperatively, the PACU (postanesthesia care unit) nurse and/or floor nurse administers the postoperative doses until the patient is discharged home. Although it was not required as part of our pilot, patients were given information to continue treatment at home if desired. The most important piece is to get the nasal sanitizer done preoperatively because that is where all the data and the research are strongest around efficacy and SSI prevention.
Another key thing we did was to add the documentation of administration on the medical administration record (MAR) in the EHR. Even though nasal sanitizer is not a medication, we were able to convince the pharmacy to add it to the MAR so nurses had a way to document it and ensure the patient received it. We know nurses are compliant with medication administration, so adding this to the MAR allowed us to monitor and measure compliance.
Q: Can you tell us about the process of getting multiple stakeholders on board?
Yfantis: Our core team was perioperative nursing (listed on our poster) and the antibiotic stewardship team, which includes our epidemiologist physician champion and our antibiotic stewardship pharmacist. Additionally, the perioperative educator, perioperative documentation specialist, infection prevention, and supply chain and value analysis were essential parts of our team.
The value analysis team was instrumental in assisting us with obtaining approvals for new product introduction and purchasing. We also needed approval from the Department of Surgery and buy-in from the Medical Executive Committee, Nursing Administration, and the Hospital Executive Leadership. Everything went remarkably smoothly. Logistically, we were lucky to have a pharmacy colleague on our team, which helped tremendously with the IT changes we requested. Getting nasal sanitizer added to the MAR allowed us to create and run reports to evaluate and measure compliance, which was extremely helpful. Thankfully, the amazing support we had from executive leadership helped expedite the EHR changes and allowed our pilot to progress without barriers.
Q: What are the big takeaways from this project?
Yfantis: One big thing we learned, which we already knew, is that nurses are consistent and exceptionally reliable change agents. Using an NIPO and adding the nasal sanitizer to the MAR were vital to successful nurse administration compliance and to the integration into everyday practice.
This pilot has brought nasal decolonization to the forefront in the preoperative nurse's mind equal to CHG bathing and reinforced it into a routine. Suburban Hospital nurses tend to be early adopters and very progressive in accepting evidence-based quality improvement initiatives.
Q: What’s next?
Yfantis: The positive effects on SSI rates and administration compliance has led our organization to permanently add nasal sanitizer to our supply chain. We have also extended the protocol to include other high-risk populations (eg, cardiac surgery). Also, the results of our pilot inspired the ICU to implement their own pilot of nasal sanitizer for the reduction of MRSA and CLABSI (central line associated blood septicemia infection). The ICU experienced dramatic improvement in both since initiating their pilot. There is now talk of extending nasal sanitizer to the IMCU, Cath Lab patients, and other populations who may benefit from it.
The exciting news is that we have managed to influence change at the system level. Suburban Hospital, part of Johns Hopkins Medicine, was a driving force behind adding nasal decolonization to the EHR, namely the preoperative checklist. That is a big deal when one considers that assessing patients’ preoperative nasal decolonization status is now hardwired into the preoperative assessment, mitigating the risk of missing a crucial step in SSI prevention.
But the one thing that we are most proud of from our pilot is that we now have a nurse-driven intervention that engages and involves the patient in SSI prevention, and that ultimately has a positive impact on outcomes for the patients, providers, and nurses.