Efforts to repeal and replace the Affordable Care Act (ACA) are ongoing, with continued uncertainty about what may happen and when. To keep things in perspective, here’s a snapshot of recent developments. On May 4, the US House of Representatives approved the American Health Care Act (AHCA) by a vote…
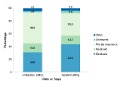
Editor's Note According to statistics from the Agency for Healthcare Research and Quality (AHRQ), in 2014, 17.2 million hospital visits (inpatient and outpatient) included surgical procedures. More than half (57.8%) occurred in a hospital-owned outpatient surgery setting, and the remaining (42.2%) were inpatient. Private insurance was the primary payer for…

Editor's Note The US House of Representatives on May 4 passed the American Health Care Act with 217 yes votes; 216 was the number needed. The bill now moves to the Senate. The House Republicans passed the American Health Care Act with a slim majority on Thursday. The bill gives…

Editor's Note The 123-page bill, called the “American Health Care Act,” was released March 6, Modern Healthcare reports. The bill replaces the Affordable Care Act’s (ACA’s) income-based premium tax credits with age-based tax credits. It also enhances federal funding for states to expand Medicaid to low-income adults, and it converts…
Editor's Note Despite the Affordable Care Act, which was designed to improve access to care for patients without insurance, patients without insurance have lower use of high-quality hospitals, this study finds. The probability of admission to high-quality hospitals was similar for patients with Medicaid (23.3%) and private insurance (23.0%), but…
Healthcare consumers and providers alike are watching to see what changes will occur under the administration of President-elect Donald Trump. Thus far, at least a partial repeal of the Affordable Care Act (ACA) seems likely. That’s in part because US Rep Tom Price (R-GA) is Trump’s pick for Health and…
Editor's Note Medicare Advantage plans paid hospitals 8% less for hospital services than fee-for-service Medicare in 2009 and 2012, finds this study. Researchers also found that commercial insurers paid hospitals much higher than Medicare Advantage or fee-for-service Medicare. Some of this difference is because of higher prices commercial plans pay…
Despite warnings of calamities, implementation of the International Classification of Diseases (ICD)-10 on October 1, 2015, proceeded smoothly, with minimal impact on denied claims. In the fourth quarter of 2015, the percentage of Medicare claims denied was 10%, comparable to the preimplementation figure of 9.9%. But that doesn’t mean OR…
Editor's Note The Centers for Medicare & Medicaid Services (CMS) and Food and Drug Administration (FDA) are recommending using unique device identifiers (UDIs) in universal health insurance claims forms to improve value-based reimbursement for medical devices and postmarket surveillance, the July 14 Modern Healthcare reports. Proponents say UDIs could help…
Editor's Note June was the worst month of 2016 for healthcare information security, with 29 breaches that affected more than 11 million patient records, the July 7 Healthcare IT News reports. A total of 24 healthcare providers accounted for 86% of the breaches, with three occurring at health plans and…